Medicare Now Covers Less Invasive Colorectal Cancer Tests
(NewsUSA) - Expanded Screening Coverage Can Reduce Needless Deaths
- Expanded Screening Coverage Can Reduce Needless Deaths
Colorectal cancer deaths are declining, but shocking regional, racial and ethnic disparities remain. According to the American Cancer Society, Latinos in the United States are more likely to die from colorectal cancer than those in many Central and South American countries, and death rates among Black men and women are 40% higher than their white counterparts. Rural residents are also far more likely to die from this often-preventable disease than those in urban areas. Much of this is due to lack of screening.
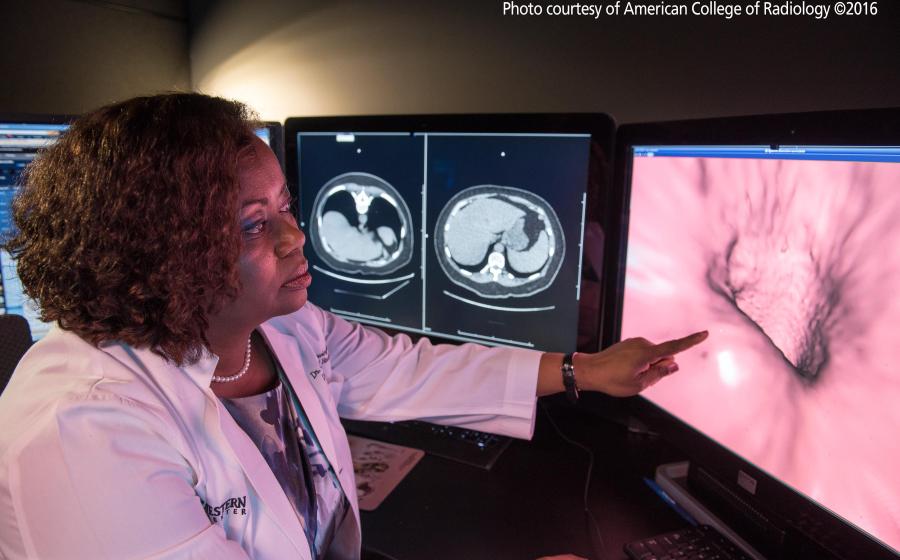
Colorectal cancer care groups, minority healthcare advocates and doctors have long held that virtual colonoscopy, or CT Colonography, can overcome cultural stigmas and anxiety associated with this screening. In January, Medicare began covering virtual colonoscopy – which uses a CT scanner to generate 3D, moving images of the colon that doctors examine for signs of cancer and for precancerous polyps, which can be removed before they become cancers.
“Patients should have a choice in their screening options,” said Anjee Davis, MPPA, CEO of Fight Colorectal Cancer. “It’s important to consider the whole patient—their preferences, comfort, and what they feel is the best fit for them. For some, it might be a virtual colonoscopy or another less-invasive screening option.”
At least 53,000 people in the U.S. still die from colorectal cancer each year. Virtual colonoscopy use is growing most quickly among Black Americans and Latinos. Many experts think more covered exams can convince the 30% of US residents who should be screened, but choose not to, to get tested.
“Affordability and accessibility are critical factors in determining whether a person will get screened for colorectal cancer. Improving access and choice for more people can help save lives and bring us closer to ending the disease in our lifetime," said Michael Sapienza, CEO of the Colorectal Cancer Alliance.
The Affordable Care Act requires private insurers to cover the exam. CIGNA, UnitedHealthcare, Anthem Blue Cross Blue Shield, Aetna and other large insurers have covered these tests for years.
Preparation for virtual and standard colonoscopies is the same, but the virtual test is far less invasive and does not require sedation. It is over in minutes. A person does not need to get a ride to or from the exam and can return to daily activities.
“Many in low-income communities, including single parents, can’t afford to take a day off work, and may not have reliable transportation or childcare,” said Cecelia Brewington, MD, Chair of Medical Imaging at Ochsner Health System, New Orleans. “Being able to go back to work afterward may determine whether that person gets tested – which can ultimately save their life.
Virtual colonoscopy is recommended by the American Cancer Society for those at average colorectal cancer risk, with no family history of the disease or other major gastrointestinal issues. President Obama had a virtual colonoscopy while in office.
“Medicare covering virtual colonoscopies enables more people to be screened, allows doctors to remove more polyps before they become cancers and helps people avoid getting this disease altogether. This will save lives,” said Judy Yee, MD, chair of the American College of Radiology Colon Cancer Committee, and Professor and Chair of Radiology at Montefiore Health System and Albert Einstein College of Medicine, Bronx, NY.
Those ages 45 and older should talk to their doctor about which exam works best for them.
More information is available at RadiologyInfo.org/virtualct.


 - Aunque las enfermedades del corazón se pueden prevenir en gran medida, aun así, siguen siendo la principal causa de muerte en los Estados Unidos. Las enfermedades cardíacas afectan a millones de personas y su impacto no es igual en todas las comunidades.
- Aunque las enfermedades del corazón se pueden prevenir en gran medida, aun así, siguen siendo la principal causa de muerte en los Estados Unidos. Las enfermedades cardíacas afectan a millones de personas y su impacto no es igual en todas las comunidades.
 - Heart disease is largely preventable, yet it’s still the leading cause of death in the United States. It affects millions of people, and its impact is not shared equally among all communities.
- Heart disease is largely preventable, yet it’s still the leading cause of death in the United States. It affects millions of people, and its impact is not shared equally among all communities.
 - A Convenient New Approach to Metabolic Health
- A Convenient New Approach to Metabolic Health
 - Today, millions of Americans live with undetected hypertension, unaware that it can impact even the healthiest of individuals — a lesson that Naomi Saucer* would come to learn firsthand. 1-2
- Today, millions of Americans live with undetected hypertension, unaware that it can impact even the healthiest of individuals — a lesson that Naomi Saucer* would come to learn firsthand. 1-2 “The Symplicity procedure was one of the best things I could have done for myself,” said Naomi. “The recovery wasn’t bad— honestly, the hardest part was having to take it easy for eight hours afterward, since I’m always on the go!”
“The Symplicity procedure was one of the best things I could have done for myself,” said Naomi. “The recovery wasn’t bad— honestly, the hardest part was having to take it easy for eight hours afterward, since I’m always on the go!”
 - Those who suffer from eye infections that threaten a person’s vision have a new treatment option that is noninvasive and counters the problem of antibiotic resistance, based on recent research and clinical work.
- Those who suffer from eye infections that threaten a person’s vision have a new treatment option that is noninvasive and counters the problem of antibiotic resistance, based on recent research and clinical work.
 - Every 2 seconds, someone in the United States needs blood, and a single donation can save lives. Shortages in the nation’s blood supply can happen any time. Donors, especially those who donate regularly, keep our blood supply stable.
- Every 2 seconds, someone in the United States needs blood, and a single donation can save lives. Shortages in the nation’s blood supply can happen any time. Donors, especially those who donate regularly, keep our blood supply stable. - Cada 2 segundos, alguna persona en los Estados Unidos necesita sangre. Una sola donación puede salvar vidas. En cualquier momento se puede presentar escasez en el suministro de sangre del país.
- Cada 2 segundos, alguna persona en los Estados Unidos necesita sangre. Una sola donación puede salvar vidas. En cualquier momento se puede presentar escasez en el suministro de sangre del país.
 - We take X-rays for granted, but they were unknown until German physicist Wilhelm Roentgen discovered them 130 years ago. Today, they’re associated with detecting problems with bones, teeth, and more, but one of their most important uses is curing common skin cancer.
- We take X-rays for granted, but they were unknown until German physicist Wilhelm Roentgen discovered them 130 years ago. Today, they’re associated with detecting problems with bones, teeth, and more, but one of their most important uses is curing common skin cancer.
 - Diabetes remains a growing health crisis in the United States, but many people living with diabetes are confused as to which foods should be part of their meal plan, according to the American Diabetes Association (ADA). For example, many people believe that those with diabetes or prediabetes should avoid potatoes, but in fact potatoes are highly nutritious and can be part of any healthy diet.
- Diabetes remains a growing health crisis in the United States, but many people living with diabetes are confused as to which foods should be part of their meal plan, according to the American Diabetes Association (ADA). For example, many people believe that those with diabetes or prediabetes should avoid potatoes, but in fact potatoes are highly nutritious and can be part of any healthy diet. 

